April 2024
Opioid Prescribing
Table of Contents




About Our Issue
The discourse surrounding opioid therapy continues to be heated. Complex regulations and guidelines and concerns about medication misuse are pitted against ensuring those with chronic pain have reasonable access to the correct medical interventions to manage their symptoms.
An increasing number of states require opioid prescribing or pain management education as part of their medical licensing requirements. Because of this, ProAssurance continues to make providing resources on this topic a priority. This includes providing CME options for our insureds that help them to meet their licensing requirements—as well as providing you with resources to stay up-to-date with the current regulations and requirements so you may speak on the topic in your sales conversations.
Our main effort in this area is our "Opioid Treatment" Loss Prevention Seminar, released last month. In addition to being available for CME, this program is an option to earn risk management premium credit. This program addresses common challenges faced by physicians and other prescribers who manage patients with acute and chronic pain or treat substance use disorders.
We have also assembled a variety of risk management materials and industry news on opioid prescribing requirements for those who would like to enhance their education.
We are always open to your suggestions regarding industry topics that would be helpful for us to cover. If you have a topic you would like us to add to our ProVisions editorial calendar, email AskMarketing@ProAssurance.com. Thank you.

Opioid Treatment
 The 2024 physician Loss Prevention Seminar (LPS), “Opioid Treatment: Guidelines, Research, and Prescribing,” addresses common challenges faced by physicians and other prescribers who manage patients with acute and chronic pain and treat substance use disorders. This activity reviews potential approaches to opioid-based pharmacology and opioid therapy. Faculty members discuss the risks of opioid treatment, provide practical and applicable insights to safely manage patients, and assist in navigating the complexities of agency regulations and guidelines.
The 2024 physician Loss Prevention Seminar (LPS), “Opioid Treatment: Guidelines, Research, and Prescribing,” addresses common challenges faced by physicians and other prescribers who manage patients with acute and chronic pain and treat substance use disorders. This activity reviews potential approaches to opioid-based pharmacology and opioid therapy. Faculty members discuss the risks of opioid treatment, provide practical and applicable insights to safely manage patients, and assist in navigating the complexities of agency regulations and guidelines.
This online-only seminar takes about two hours to complete and is divided into multiple segments, so your clients can watch the full program in multiple sittings. It qualifies for continuing medical education (CME) credit upon successful completion of the post-test.
Course Objectives & CME
 This seminar is intended for physicians of all specialties, physician assistants, CRNAs, and nurse practitioners; no experiential or academic prerequisites are necessary. Objectives include:
This seminar is intended for physicians of all specialties, physician assistants, CRNAs, and nurse practitioners; no experiential or academic prerequisites are necessary. Objectives include:
- Identify and mitigate the primary risks associated with prescribing opioid medications.
- Evaluate current processes and incorporate best practice guidelines.
- Apply risk reduction strategies to reduce potential patient harm and professional liability claims.
This online-only seminar takes about two hours to complete and is divided into multiple segments, so your clients can watch the full program in multiple sittings. It qualifies for continuing medical education (CME) credit upon successful completion of the post-test.
Potential Policy Discount
 Participation in this loss prevention seminar may qualify ProAssurance physicians for a premium credit if they attend the entire two-hour activity and pass the post-test with a score of 75% or greater. Premium credits are subject to approval by the state insurance department and are applied at policy renewal.
Participation in this loss prevention seminar may qualify ProAssurance physicians for a premium credit if they attend the entire two-hour activity and pass the post-test with a score of 75% or greater. Premium credits are subject to approval by the state insurance department and are applied at policy renewal.
To take the seminar, insureds should sign in to the secure services portal at the top of any page of ProAssurance.com. From there they select “Physician Online Seminars” from the Seminars menu.
Visit RiskManagement.ProAssurance.com/LPS for more information.
2024 ProAssurance Practice Administrator Seminar
 The Risk Management team is releasing the 2024 Practice Administrator’s Seminar. This year’s seminar addresses the evolving legal and risk landscape in relation to controlled substance prescribing. You can join them as they provide risk mitigation strategies from an operational perspective. The seminar will feature medical professional liability topics including proper screening and monitoring techniques, polypharmacy, medical record documentation, the process of considering nonpharmaceutical pain management strategies, and when to consult with or refer to other specialists. This seminar is set to be released later this year.
The Risk Management team is releasing the 2024 Practice Administrator’s Seminar. This year’s seminar addresses the evolving legal and risk landscape in relation to controlled substance prescribing. You can join them as they provide risk mitigation strategies from an operational perspective. The seminar will feature medical professional liability topics including proper screening and monitoring techniques, polypharmacy, medical record documentation, the process of considering nonpharmaceutical pain management strategies, and when to consult with or refer to other specialists. This seminar is set to be released later this year.
The current Practice Administrator Seminar is available until June 2024. This seminar addresses the baseline self-assessment, provides practical solutions to help evaluate common risks, and helps develop a process to keep a practice on track. The seminar is two hours and can be found here.

Sure Med Expands to Work with Implanted Technology
 In 2023 ProAssurance partnered with Sure Med Compliance to offer the only digital health platform, called Perspectives in Care, scientifically validated to mitigate risk to both patient and provider in pain management settings. It can be difficult to balance treating a patient’s pain while also taking crucial steps to avoid misuse, abuse, dependence, and overdose of opioids. Providers must recognize “red flags” and signals of misuse. By delivering clinical insights that help influence safer prescribing decisions, Sure Med helps protect healthcare providers from liability and allow doctors to create safer exposures to controlled substances.
In 2023 ProAssurance partnered with Sure Med Compliance to offer the only digital health platform, called Perspectives in Care, scientifically validated to mitigate risk to both patient and provider in pain management settings. It can be difficult to balance treating a patient’s pain while also taking crucial steps to avoid misuse, abuse, dependence, and overdose of opioids. Providers must recognize “red flags” and signals of misuse. By delivering clinical insights that help influence safer prescribing decisions, Sure Med helps protect healthcare providers from liability and allow doctors to create safer exposures to controlled substances.
Sure Med recently announced its exclusive partnership with Curonix LLC, a medical technology company dedicated to easing chronic pain without the use of opioids, to collect clinical data from a nerve stimulating implanted device.
Pain Management Without Opioids
Curonix’s Freedom® Peripheral Nerve Stimulation (PNS) provides lasting chronic pain relief through a non-opioid, minimally invasive implanted technology. Paired with Sure Med’s digital health platform, Curonix will work with physicians and their teams to collect and analyze PNS data to expand the body of clinical evidence to further support PNS efficacy.
“Access to opioid sparing modalities is becoming increasingly limited,” says John Bowman, founder and CEO of Sure Med Compliance. “Coinciding with this industry challenge is another reduction by the DEA in aggregate production quotas of opioids. This scenario is creating an environment in which patients with chronic, intractable pain are forced to seek treatment using illegal means. Our goal in this partnership is to increase the commercial viability of products like Curonix’s Freedom stimulators, a product that has been shown to decrease pain, improve function, and decrease the amount of opioids needed to treat pain.”
Sure Med partners with forward-thinking companies like ProAssurance and Curonix to work toward solutions to help end the opioid overdose epidemic through greater compliance in pain management settings. More than 40,000 patients have already enrolled in Sure Med’s Perspectives in Care program.
It is available to ProAssurance insureds at no additional cost.
For more information, visit SureMedCompliance.com.

Opioid Prescribing: Behind the Numbers
According to the Centers for Disease Control & Prevention, millions of Americans who suffer from pain are often prescribed opioids to treat their conditions. The result has been a growing problem of opioid use disorder and overdose.
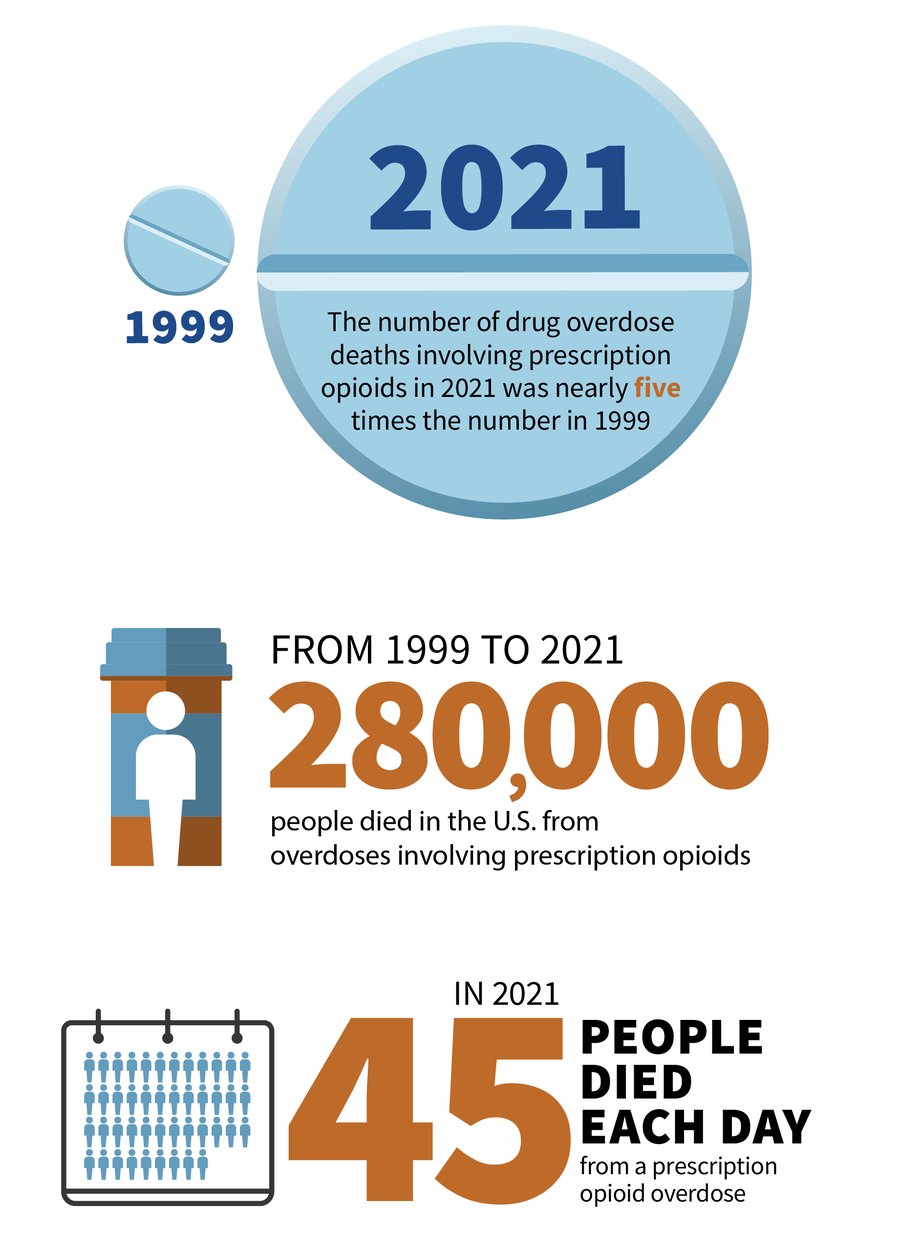
Since the 1990s, when the amount of opioids prescribed to patients began to grow, the number of overdoses from prescription opioids has also increased. Even as the amount of opioids prescribed and sold for pain has increased, the amount of pain reported has not similarly changed and the number of deaths have increased dramatically.
In fact the number of drug overdose deaths involving prescription opioids in 2021 was nearly five times the number in 1999.
In 2021, 45 people died each day from a prescription opioid overdose, totaling nearly 17,000 deaths. Prescription opioids were involved in nearly 21% of all opioid overdose deaths in 2021. From 1999 to 2021, nearly 280,000 people died in the U.S. from overdoses involving prescription opioids.
A review of our closed claims over the past 10 years indicates that claims involving opioid therapy in chronic pain management patients generally involve overdose deaths. Allegations supporting negligence claims against physicians include excessive opioid prescribing; failure to refer the patient for pain management, addiction, or behavioral health treatment; failure to discover the patient was “doctor shopping”; failure to recognize suicide risk; and negligent tapering.

ProAssurance Risk Management Opioid Prescribing Resources
Clinicians are responsible for the safety of the patients for whom they prescribe opioid pain medications. There are no shortcuts to reducing the risk of accidental and intentional overdose. These patients require various assessments, treatment plans that maximize the use of non-opioid treatments, monitoring, and referral when appropriate. A thorough informed consent process that covers the risks associated with opioid use, the expected benefits, uncertainties of the anticipated treatment plan, and the alternatives is an essential aspect of pain management that includes opioid therapy.
ProAssurance Risk Management has a wealth of resources to help practices increase patient safety and maintain compliance when prescribing opioids. ProAssurance insureds can contact a Risk Management consultant at 844-223-9648 or email RiskAdvisor@ProAssurance.com to discuss risk reduction strategies for responsible prescribing practices and keeping patients safe.
Opioid Prescribing Resources
Loss Prevention Seminar 2024: Opioid Treatment: Guidelines, Research, and Prescribing
This program addresses common challenges faced by physicians and other prescribers who manage patients with acute and chronic pain or treat substance use disorders. This activity reviews potential approaches to opioid-based pharmacology and opioid therapy. Join us as faculty members discuss the risks of opioid treatment, provide practical and applicable insights to safely manage patients, and assist in navigating the complexities of agency regulations and guidelines.
2024 Practice Administrator's Seminar (PAS): Opioid Prescribing: Minimize the Risks to Patients and Physicians (scheduled release July 1, 2024)
This course addresses the shared challenges faced by practice administrators when a physician or other healthcare professional recommends a treatment plan that includes the prescribing of opioid medications to a patient. Join us as we discuss the inherent patient safety and medical professional liability risks associated with the care and treatment of chronic pain patients in the physician office practice setting.
Online Seminar: Opioid Prescribing: Keeping Patients Safe
This healthcare risk management online seminar will focus on the opioid crisis and the impact of opioid prescribing on patient safety. The discussion will include closed claims and risk reduction strategies you may implement to mitigate your liability exposure and increase patient safety.
Opioid Prescribing for Chronic Pain
Case Study: Reducing Opioid Overdose Risk in Patients with Opioid Use Disorder
Case Study: Optimizing Opioid Therapy for Patients with Behavioral Health Disorders
Case Study: Strategies for Tapering Patients off Long-Term Opioid Therapy
Best Practices: Strategies for Managing Drug-Seeking Patients
CME Requirements for Opioid Prescribing and Pain Management by State
Many states have instituted new regulations in response to the current opioid crisis, with medical licensing boards updating their continuing medical education (CME) requirements. Medical professionals may need to complete activities related to pain management and safe opioid prescribing to fulfill their credits. CME requirements vary by state, as do specifications regarding hours and topics, and any updates may be found by visiting your state's medical board website.
There are currently no CME requirements for pain management and opioid prescribing in Hawaii, South Dakota, and Wyoming. For more state-specific information, read Pain Management & Opioid CME Requirements by State (BoardVitals, January 24, 2024).

*every two years
States with Other Specific Requirements
- The Delaware Board of Medical Licensure and Discipline requires physicians to undergo two credit hours in controlled substance prescribing practices, treatment of chronic pain, or topics related to controlled substances.
- One credit hour on Delaware Law pertaining to prescribing and distribution of controlled substances is required within the first year of registration.
Opioid training is required for DEA-registered providers. This training meets the requirements of the Medication Access and Training Expansion (MATE) Act, which was passed as part of the Consolidated Appropriations Act of 2023.
Licensed Primary care physicians are required to complete CME focused on CDC guidelines for proper opioid prescribing.
Prescribers must complete eight hours of training on the treatment of patients with opioid or other substance use disorders.
- Physicians are required by the Kentucky Board of Medical Licensure to complete 4.5 credit hours of board-approved training related to pain management, KASPER, or addiction disorders.
- DEA-licensed prescribers of Buprenorphine-Mono-Product or Buprenorphine-Combined-with-Naloxone must complete 12 credit hours specific to addiction medicine within each three-year licensing period.
When applying for a controlled substance registration, new and renewal applicants are required to attest to completion of two credit hours related to the Prescribing or Dispensing of Controlled Substances guidelines.
All DEA-registered practitioners are required to complete a one-time eight hours of training on the treatment and management of patients with opioid or other substance use disorders. This includes the appropriate clinical use of all FDA-approved drugs for treatment of a substance use disorder.
Physician owners or operators of pain management clinics must complete at least 20 hours of training in pain medicine, including a minimum of one course addressing the potential for addiction.
The Oklahoma State Board of Osteopathic Examiners requires one credit in the prescribing of controlled substances.

Second Temporary Extension of Telemedicine Flexibilities for Prescription of Controlled Medications
The Drug Enforcement Administration (DEA), in step with the Department of Health and Human Services (HHS), put forward two notices of proposed rulemaking in March 2023 seeking comments on proposals to allow prescribing of controlled medications via telemedicine. The proposals specifically covered instances where prescribing practitioners have never conducted an in-person medical evaluation of a patient. In May of that year after initial review of the comments, the DEA and HHS issued a temporary rule continuing certain exceptions granted in March 2020 as a result of the COVID-19 pandemic. The effective period for this rule was extended to November 11, 2023, and has been further extended to December 31, 2024.
These exceptions to the Ryan Haight Online Pharmacy Consumer Protection Act of 2008 were granted in order to prevent lapses in care during the pandemic. Their flexibilities authorize practitioners to prescribe schedule II-V controlled medications to patients via audio-video telemedicine appointments, without an in-person visit prerequisite. This includes the prescription of schedule III-V narcotic controlled medications that are approved by the Food and Drug Administration for the treatment of opioid use disorder, specifically for maintenance and withdrawal management.
The purpose of these temporary regulatory changes includes preventing the reduction of care access for patients who have not been able to establish a telemedicine relationship with their practitioner pending a final rule to address telemedicine more generally. Additionally, the extensions enable sufficient time for medical professionals and patients to prepare for any future regulations that might apply to prescribing controlled medications via telemedicine.
Read the full published Rule by the DEA and HHS: “Second Temporary Extension of COVID-19 Telemedicine Flexibilities for Prescription of Controlled Medications”
.png?width=300&name=MicrosoftTeams-image%20(28).png)
To better understand how states are using Medicaid to help address the opioid epidemic, the 23rd annual Medicaid budget survey, conducted by Kaiser Family Foundation (KFF) and Health Management Associates (HMA), asked about the following specific strategies adopted or planned by state Medicaid officials for state fiscal years (SFYs) 2023 and 2024 to address the opioid epidemic: removing prior authorization for buprenorphine (a medication treatment for OUD), reimbursing for the initiation of buprenorphine treatment via telehealth, covering over-the-counter (OTC) Narcan, and implementing other initiatives. (Kaiser Family Foundation)
More than 200 virtual care stakeholders, including trade associations, healthcare providers, and telehealth companies, have signed a letter urging the United States Drug Enforcement Administration (DEA) to release a revised proposed rule allowing virtual prescribing of controlled substances soon. The letter states that a revised rule permanently allowing controlled substances to be prescribed via telehealth without a prior in-person examination “is crucial for access to mental health, substance use disorder, and other telehealth care.” (mHealth Intelligence)
Some members of Congress are demanding federal oversight of billions of dollars in opioid settlements, which state and local governments began spending over the past two years—with some using it to plug budget holes rather than fight the addiction crisis. (NPR)
Opioid prescriptions by volume declined by 12% in 2017, the largest single-year change in a quarter of a century, according to a report from the Iqvia Institute for Human Data Science. That number is based on prescriptions by morphine milligram equivalents, a metric that takes into account the strength and dosage of drugs, but the total number of filled opioid prescriptions also dropped by 10.2% per month, according to the report. Prescriptions for high-dose opioids were filled even less frequently, with a 16.1% decline. (Fortune, via AOL)
A group of 31 physicians and researchers called on the FDA to reverse its decision about AvertD, a test that uses DNA to identify whether adults may have an elevated risk of developing opioid use disorder (OUD). In a letter to FDA Commissioner Robert Califf, MD, experts in genetics, addiction, psychiatry, public health, and device regulation asked the agency to revoke its recent approval of AvertD, based on research that doesn't support the methodology used by the test's sponsor. (MedPage Today)

Overcoming Client Sticker Shock

The renewal notice for my homeowner's insurance hits my mailbox each September. However, this past year, Gloria, my insurance agent, called me preemptively. She began, "We need to discuss your renewal." My pulse started to race. I knew what was coming. Living in Florida means grappling with soaring home insurance rates. By 2023, numerous insurers had left the state with the remaining companies only one hurricane (or other catastrophic event) away from saying adios too. I didn't expect this to be a pleasant conversation.
Renewal and Reality
Gloria's update wasn't entirely bleak: "You're one of the lucky ones. Your insurer stopped issuing new policies and will only renew some existing ones. You made the cut, which is good news since the remaining insurers in the state wouldn’t quote, except for the state-run non-profit insurer of last resort." I braced as Gloria revealed what this call was really about—the premium. I gasped. It almost doubled to an amount eclipsing the mortgage payment on my first house. Gloria was empathetic, but it was one of those it-is-what-it-is moments.
Defending Product Price Increases in Healthcare
I had countless similar conversations with my MedTech accounts. Cost containment is an issue HCPs must confront with almost every decision. When accounts receive notifications of price increases, suppliers' phones start ringing with threats to shift business. It's not fun defending premium increases, but it comes with the territory (literally!). When clients confront premium hikes, consider these approaches:
Reality Check:
When your clients express dismay over premiums, acknowledge it. Then, review the client's options. Be empathetic like Gloria, but help them accept the reality.
Reframe:
Get clients to focus on what truly matters in a lawsuit—a solid legal defense and comprehensive liability coverage. Is a lower premium worth the increased risk to their financial present and future and reduced peace of mind?
Cost Justify:
Explain the average cost of defending a medical malpractice lawsuit and some recent jury awards in their state. Show when total costs are considered, it costs more, in the long run, to choose a cheaper premium versus ProAssurance's comprehensive coverage.
Challenge the Concept of Acceptable Coverage:
HCPs routinely default to clinically acceptable products over superior ones to contain costs. Acceptability can vanish once the client understands their actual costs during a lawsuit. Share a case study about a healthcare professional who risked lower-cost coverage and what it ultimately cost the clinician or institution.
Reinforce the Value, Including Value-added Benefits:
There's more to assessing a policy's value than comparing policy limits and premiums. Show that ProAssurance doesn't just provide a policy but a comprehensive package to help clients manage medical liability. Part of that value includes you, an agent ready to respond whenever the call comes. When comparing premiums, focus on the premium difference, not the annual premium, to provide perspective. To minimize the price difference even more, break it down to what the difference is monthly and clarify what it buys in terms of added protection.
Embracing Robust Protection: The Value Beyond Price
While clients may recoil when notified of premium hikes, understanding the reality of the situation and the value of investing in robust protection is essential. Lower premiums might seem inviting, but no healthcare professional will ever say, "I'm sure glad I bought the cheapest policy I could find," when a subpoena arrives at their door. As an agent, it's imperative to champion the unparalleled value that ProAssurance brings to the table, even in the face of rising premiums. After all, MPL coverage isn't just about financial security; it's about having confidence in your carrier and the good night's sleep that comes with it.

|
Written by Mace Horoff of Medical Sales Performance. Mace Horoff is a representative of Sales Pilot. He helps sales teams and individual representatives who sell medical devices, pharmaceuticals, biotechnology, healthcare services, and other healthcare-related products to sell more and earn more by employing a specialized healthcare system. Have a topic you’d like to see covered? Email your suggestions to AskMarketing@ProAssurance.com. |






